There are various reasons one can have ankle pain. It can range from suddenly enduring an ankle injury, or it may gradually happen from having arthritis. There are several bones, muscles, tendons, and ligaments in each ankle, and ankle pain can develop for many reasons. Tendonitis can occur when the tendons become inflamed, and this can happen to people who run frequently on uneven surfaces. It may feel worse while standing or walking, and will start to feel better with adequate rest. Achilles tendonitis is felt in the back of the ankle, and that part of the foot may feel tight in the morning after rising. An ankle fracture can cause severe pain and discomfort, and the symptoms that generally accompany this type of ankle pain are bruising, swelling, and difficult walking. Additionally, the ankle may look deformed, and it will not be possible to bend the ankle. If you have ankle pain for any reason, it is suggested that you consult with a podiatrist who can effectively diagnose and treat this type of pain.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with one of our podiatrists from Canonsburg Podiatry Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
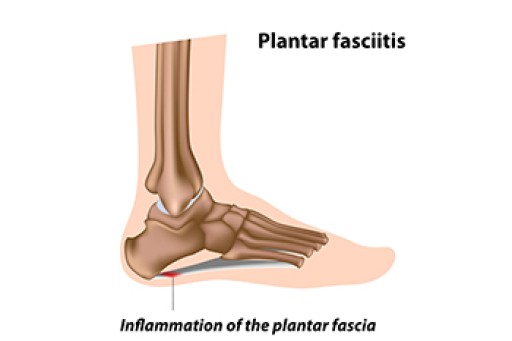
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Canonsburg and McMurray, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.