An ingrown toenail is easy to notice. The nail grows into the skin instead of over it, and it may appear red. Ingrown toenails may also become infected and bleed if prompt medical attention is not sought. This foot condition can happen from wearing shoes that are too tight or from improperly trimming the toenails. People who are born with naturally curved toenails may be prone to ingrown toenails. Temporary relief may be found when the foot is soaked in warm water and a small piece of cotton is used to gently pull the skin away from the nail. A more permanent solution is provided by a podiatrist in partially or fully removing the affected nail. This is a relatively fast procedure, but it is suggested to consult with a podiatrist to learn more. If you have developed an ingrown toenail, call your local podiatrist today.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact one of our podiatrists of Canonsburg Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
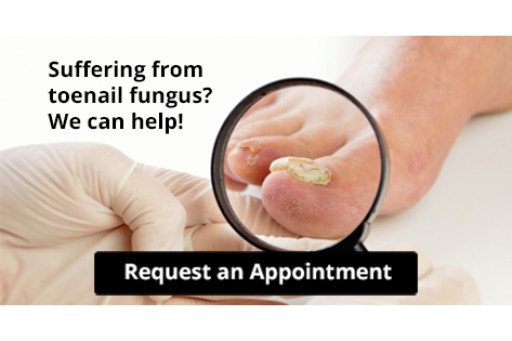
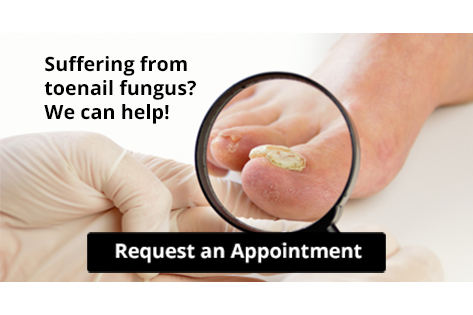
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Canonsburg and McMurray, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.